Health care executives know that how they get paid is evolving. And as part of the pressure to move towards value, they are seeking to address drivers of health (DOH) – also known as social determinants of health – as part of their care models. But what leaders may not know is that trying to address DOH from within their existing business models will be a harsh lesson in failure.
To deliver on a new value proposition such as addressing DOH, the resources and processes to sustain an organization’s financial viability must evolve as well. As a result, leaders need to completely redesign their business models – not just their profit formulas – to thrive in the future. Thankfully, leaders of traditional organizations can learn from the approaches implemented by innovators successfully addressing DOH.
As part of my research for the Institute’s health care vertical, my colleagues and I conducted a landscape scan of 84 health care entities. We then interviewed 15 organizations, targeting those with a reputation as a leader in addressing DOH, or because of their published success in improving health-related quality-of-life (QoL) or lowering care costs. We discovered those that can make an impact in DOH don’t look like traditional health care companies.
Established business models + DOH innovations = an unhealthy combination
While previous arguments have attributed failure of DOH efforts to incumbent organizations’ lack of planning, that is a misdiagnosis. These organizations fail to address DOH effectively because their business models don’t allow it.
In their 2009 HBS Module Note, “What are business models and how are they built?”, late Professor Clayton Christensen and Mark Johnson defined a business model as four interlocking elements that, when taken together, create and deliver value. These elements are value proposition, resources, processes, and profit formula/priorities. The framework is visualized for a health care business model in the image below.
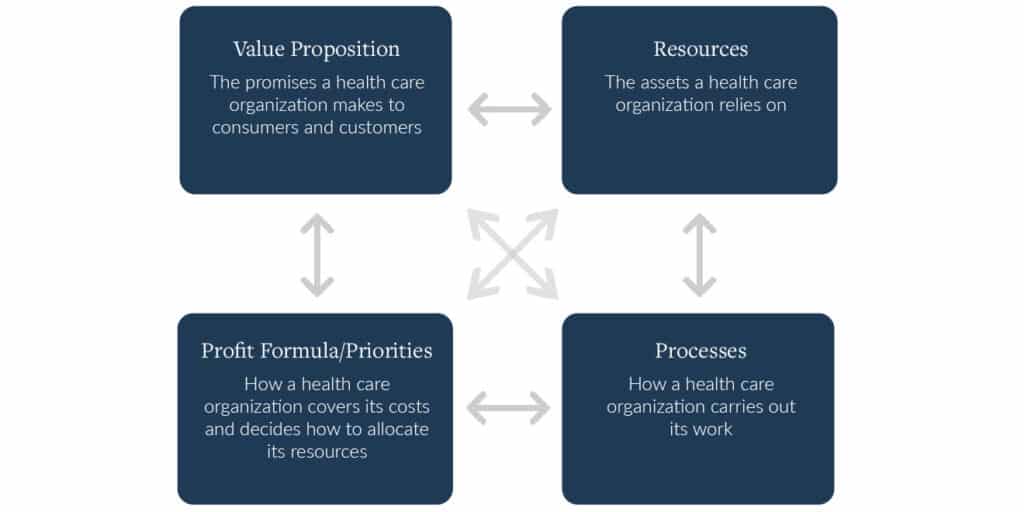
Source: This graphic was originally published in Clayton M. Christensen and Mark W. Johnson, “What Are Business Models, and How Are They Built?” Harvard Business School Module Note, August 2009 (revised November 2021). It has been modified by the author to focus on health care business models.
Business models define what an organization can and can’t do, what it must accomplish, and which innovations it can and will pursue. In an organization’s early days, all four components are flexible. But for the organization to survive and create a reliable margin, these components solidify, become increasingly interconnected and resist change. As a result, a mature organization can only successfully deliver value propositions that fit its existing resources, processes, and profit formula.
That is why established FFS models can’t easily pivot to incorporate DOH. Their resources, processes, and profit formula won’t allow for the changes required to make these innovations successful at scale. In short, leaders can’t deliver a new value proposition from within an old business model.
Four components of successful new models
In stark contrast to traditional FFS business models, our research revealed that innovators making an impact in DOH are building new business models around four key components. First, they address the consumer’s (i.e., the patient or member) and customer’s (i.e., the employer or insurer) desired progress. For example, Factor Health develops pre-clinical interventions that address payers’ pain points and consumers’ needs in the flow of people’s lives.
Their Sunshine Calls program trained lay people to have empathetic phone conversations with food-insecure seniors struggling with loneliness. The seniors decided what frequency they wanted to speak with the caller and what they would discuss. As a result of the intervention, seniors had lower loneliness, anxiety, and depression scores. And from a customer perspective, the intervention demonstrated a cost-effective approach to addressing loneliness, a risk factor for mortality and negative health outcomes, which come at higher costs than prevention.
Second, innovative organizations establish payment models that incentivize serving consumer and customer needs. For some innovators, such as Oak Street Health, this entails a profit formula supported by global capitation. In this set up, Oak Street receives a per member per month (PMPM) payment to cover a primary care patient’s complete care. If Oak Street takes care of the patient with primary and other low-acuity care avenues, they are likely to yield a positive margin. This profit model allows them to support their value proposition of keeping patients “happy, healthy, and out of the hospital.”
Others are pursuing philanthropy to support DOH efforts. Over 70% of organizations we interviewed cited private grants or philanthropic donations as a key funding source. According to interviewees, philanthropic funders are often more understanding that DOH efforts can take years to show a return, and often incentivize learning and innovation. These aligned incentives allow innovators to test, iterate, and then scale the efforts that prove cost-effective in improving health and life.
Third, innovators are measuring what matters to those they serve. Church Health, a charitable care model, provides one example. To measure the impact of their dental care services on patients’ lives, they track hourly wages before dental surgery, and up to two years afterward to capture the value of their services to consumers’ lives and economic stability.
Humana also measures success through the eyes of the consumer with the use of the CDC’s Healthy Days tool, a four-question, self-reported questionnaire where individuals assess the number of mentally and physically unhealthy days they had over the last month. In 2020, Humana’s Medicare Advantage (MA) members maintained overall QoL and improved their healthy physical days, even amid a global pandemic.
Fourth, leaders in DOH are connecting dots across the disconnected ecosystem to achieve their goals. The size and complexity of today’s DOH problem requires an ecosystem approach, and no two ecosystems look exactly alike. Jefferson Health offers an example of forming extensive partnerships to address DOH that it doesn’t serve directly. One way they do so is through the Philadelphia Collaborative for Health Equity, which was created to address health inequities and reduce health disparities in Philadelphia. The Collaborative brings together community-based organizations like those addressing housing and healthy food needs, corporate partners, and Jefferson’s health system resources. Jefferson Health is also connected to Thomas Jefferson University, which houses both the Jefferson College of Population Health and the Sidney Kimmel Medical College. These colleges train the health workforce required for the future.
Perhaps even more critical than these four business model components is the common thread supporting them all: innovative organizations’ ability to establish trust with those they serve. In traditional FFS business models, processes are optimized for efficiency to support the profit model. But to effectively address DOH, building trusted relationships with patients, customers, and partner organizations is required. Patients with higher trust in their health care providers have higher quality of life, better health behaviors, and greater satisfaction with their health care treatments. Organizations effectively addressing DOH are prioritizing trust-building as they craft their business model resources and processes.
A compass to guide transformation
Taking business model theory together with our field research, we developed a compass that leaders can follow as they redesign their business models to thrive in the future. Looking at the four business model components, leaders should consider the following:
- Value proposition: Enable consumers and customers to achieve their goals
- Resources: Harness a partnership ecosystem supported by an enabling technology platform
- Processes: Hard code an approach to creating trust
- Profit formula/priorities: Reimagine revenue streams that are tied to new, consumer- and customer-focused measures of success
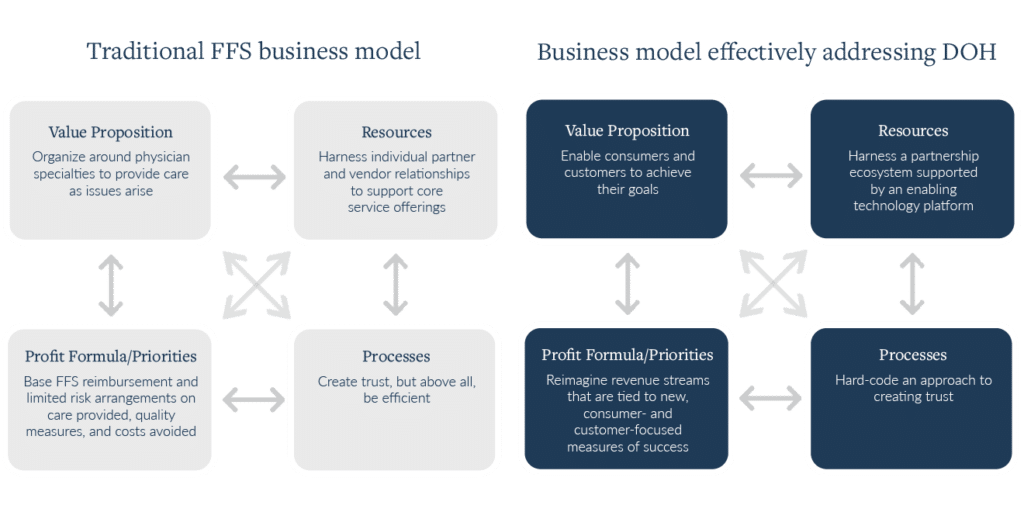
Source: Author’s analysis
Pressure to effectively address DOH and prepare for a value-based environment is here to stay. Unfortunately, today’s traditional FFS business models aren’t up for the challenge. As I’ve outlined here, leaders must transform their entire business model, not just their profit model, if they want to succeed. In the environment characterized by evolving uncertainty, leaders need a transition plan to remain financially viable and continue to serve their communities. The business model compass offered here is foundational to that plan.

