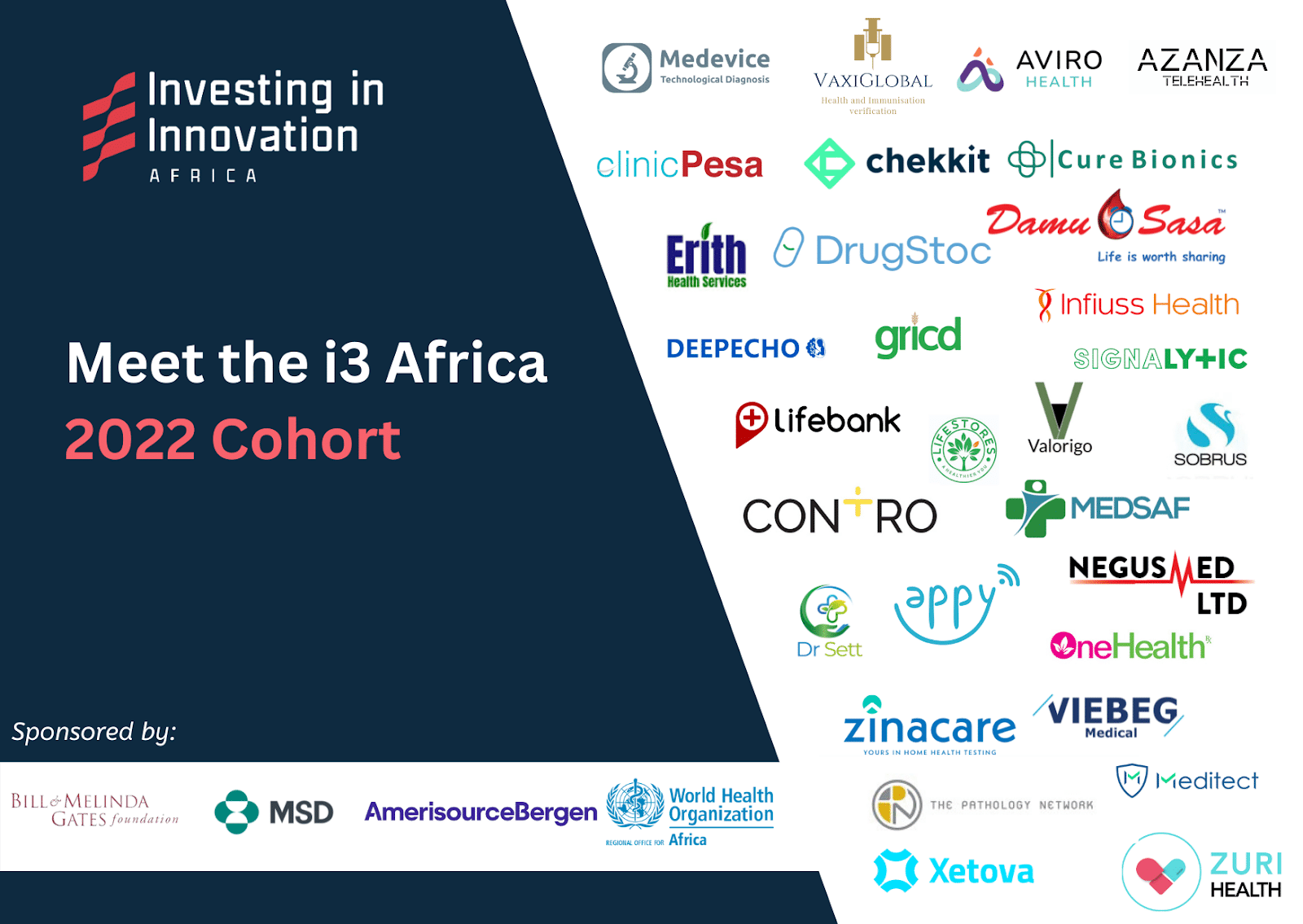
On September 26, the inaugural cohort of the Investing in Innovation (i3) program was announced (I serve on the steering committee). This group of 30 healthcare innovators–and others like them–gives Africa the best and, possibly, only chance to improve its healthcare infrastructure. If the i3 program, and others like it, succeed, African healthcare will improve. If it doesn’t, unfortunately, the state of healthcare will not only remain poor, but will always depend on the largesse of philanthropic donors or aid from foreign governments. And surely, dependence cannot be the goal of development.
The state of Africa’s healthcare system is somewhere between broken and nonexistent
Several years ago, a middle-aged man–we’ll call him John–in an African country experienced an emergency at night. John’s family rushed him to the closest hospital they could find. Upon reaching, they learned the doctor wasn’t available. Quickly, they packed their belongings and hurried to another hospital. At hospital #2, they were told the necessary diagnostic equipment to perform tests on John was not available. Like a scene from a tragic movie, their loss of hope was palpable. Dejection and despair took over as they felt John–their father, brother, and husband–slowly slip away. John’s family tried a third hospital but, by then, too much time had passed.
John lost his life at hospital #3.
If John’s story were an anomaly, it would still be too much to bear. But the fact that his story is the norm in Africa is both heartbreaking and unconscionable.
Similar to John’s story, today, most Africans don’t have access to enough skilled healthcare professionals, and up-to-date facilities and quality medicines are hard to come by.
Many illnesses are diagnosed too late–if they are diagnosed at all–and preventable diseases are still killing hundreds of thousands of people annually. When the broken healthcare system does see patients, getting access to medicines necessary to improve health is challenging as the vast majority of drugs are produced outside the continent. This increases cost and complicates supply chain issues.
Too many Africans are living on borrowed time.
Governments across Africa are working to improve Africa’s healthcare infrastructure. With limited budgets however, they are struggling to make real progress.
Consider this. The average African government spends around $650 per African annually, on everything. The $650 covers the government’s expenditures on healthcare, education, infrastructure, defense, and governance. Sierra Leone, Nigeria, and Kenya spend approximately $120, $200, and $400 respectively. It is from this budget that African governments must carve out a measly sum for healthcare.
For comparison, the United States, Switzerland, and Norway spend $29,500, $30,000, and $37,500 respectively.
Even if African governments invested efficiently, they would still not have enough resources to fix the major issues that plague their healthcare systems.
This is where the power of market-creating innovations and programs like i3 can play a significant role.
Market-creating innovations transform complicated and expensive products–like medicines–into simple and affordable ones making them accessible to many more people in society. These innovations are unique in their ability to trigger economic prosperity at scale.
The first cohort of i3 companies are focused on creating new markets and expanding existing ones in the healthcare supply chain sector. The companies are either in the early or growth phase of their development. If given the necessary capital and connections to markets and suppliers, these organizations will transform Africa’s healthcare system for the better. This is exactly what i3 hopes to provide these companies.
Even without it, some of the companies are forging ahead. For example, in Nigeria, Lifestores Healthcare democratizes access to medical services and medications through a digital marketplace that enables pharmacies and hospitals to pool their procurement needs to access genuine medications more affordably. If Lifestores scales across Africa, it will make medicines even more affordable.
In Kenya, Zuri Health is facilitating remote access to healthcare services by offering teleconsultations, appointment booking, and at-home diagnostics services. The company also provides a platform for its users to order medications and locate pharmacies on its platform.
And LifeBank, with operations in Nigeria, Kenya, and Ethiopia, enables last-mile delivery of critical health supplies, including blood, oxygen, medical consumables, and equipment to hospitals and providers. The company is leveraging a digital marketplace and an efficient distribution network to guarantee fast and convenient access to critical products.
The 30 companies in the cohort have the potential to grow into pan-African behemoths that will not only improve healthcare for the average African, but will also build Africa’s much needed healthcare infrastructure.
The Ghanaian healthcare company, mPharma, serves as an example of the kind of impact these companies can have in Africa. Less than a decade old, mPharma has grown to serve more than two million Africans annually with pharmacies and primary care consultations. The company employs more than 1,000 people, partners with over 1,000 hospitals, and generates close to $4 million in taxes annually. These innovative companies give Africa the best shot at fixing its healthcare infrastructure.
The COVID-19 pandemic exposed the vulnerability of Africa’s healthcare infrastructure. We have an opportunity to fundamentally change the paradigm on how we fix this problem. The i3 program is just the beginning.

